For years, people working with dairy cows have called the drop in calcium around calving milk fever. Ironically, milk fever, also known as hypocalcemia, does not cause a fever at all.
Gary Oetzel, D.V.M., a professor for the University of Wisconsin-Madison’s School of Veterinary Medicine, shared that detail and more during the September Hoard’s Dairyman monthly webinar. He started out by defining the two types of hypocalcemia: clinical and subclinical.
Clinical milk fever cases are cows that are recumbent or that soon will be, he noted. Meanwhile, subclinical hypocalcemic cows show minimal, nonprogressive clinical signs. Many older cows develop some level of subclinical hypocalcemia (SCH), but it is most harmful if it persists past 48 hours postcalving, he said.
A sudden depletion in blood calcium is what triggers hypocalcemia. “Calcium homeostasis is fragile around calving time. It is a difficult time metabolically for a cow,” Oetzel said.
He explained that milk is really high in calcium. For a human, 30% of the daily requirement for calcium is contained in just one cup of milk.
At calving, cows are pumping this calcium into their milk to support skeletal growth of the calf. At the same time, “They are putting themselves at great risk to secrete that much calcium,” Oetzel said.
What’s more, colostrum has twice as much calcium as regular milk. There is 0.8 to 1 gram of calcium in 1 pound of colostrum compared to 0.5 gram of calcium per pound of milk.
“This is a real shock to a cow’s system,” Oetzel explained. A cow provides some calcium during pregnancy to develop the fetal skeleton, but in the 12 hours before birth, a tremendous amount of calcium must go into colostrum. A cow then repeats that process 12 hours later. In the first 24 hours, the calcium outflow can be 20 to 30 grams.
A cow continues to pump out calcium as it reaches peak milk. “This really puts a strain on the cow,” Oetzel said. “Cows are going to struggle with calcium balance after calving just like they struggle with energy balance.”
He encouraged listeners to not take a cow’s ability to mobilize calcium for granted. “We think of cows as being amazing energy athletes, but they are also calcium athletes,” he said.
The calcium source
How do cows get the calcium they need? It’s a process known as lactational osteoporosis.
Oetzel said cows lose 9% to 13% of their skeletal calcium within the first 30 days in milk. In all, about 2.5 pounds of calcium are lost from the 21 pounds available in their bones.
“The skeletal store of calcium is sufficient,” Oetzel explained, “but it takes several days to activate the mechanisms.” That is why cows find themselves in a calcium deficiency.
Oetzel said normal blood calcium concentrations are very low, between 8.6 to 11 mg/dL (85 to 100 parts per million, ppm). Normal ionized blood calcium is about 4 to 5 mg/dL (40 to 50 ppm). For comparison, U.S. drinking water averages 51 ppm of calcium. Low blood calcium levels leave cows susceptible to clinical or subclinical hypocalcemia.
Prevention is worthwhile
The good news, Oetzel shared, is that cases of clinical milk fever are declining. Looking at National Animal Health Monitoring System (NAHMS) data, in 2002, 6.2% of cows had clinical hypocalcemia. By 2014, that number was down to 3.7%. He said a current reasonable herd goal is 2% clinical cases, and that some farms are down to less than half of a percent.
“We’ve done some really good things in reducing the risk for clinical milk fever in our dairy herds. Let’s keep it up,” Oetzel encouraged.
Even though the risk is low, Oetzel reminded the audience that the outcomes can be very bad. “Just because a cow gets up after we deliver intravenous (IV) calcium to them doesn’t mean everything is okay,” he said.
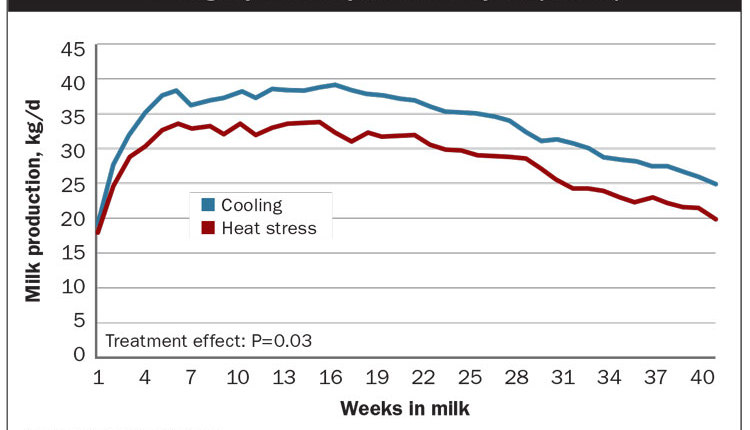
Cows that experience clinical hypocalcemia are at a greater risk for other health issues, including displaced abomasums. Herd removal is almost two times greater, and cows with clinical hypocalcemia can lose up to 14% of milk production throughout an entire lactation.
“I can’t think of any other disease that affects a cow’s production that much,” he said.
Cows that don’t show clinical signs still experience a drop in blood calcium levels and fall into the subclincal hypocalcemic category. While there is more to be learned about the subclinical form of the disease, it is well documented that the risk goes up as cows proceed through age and lactations.
“Older cows give more milk and cannot mobilize calcium as readily from their skeleton, so they are at a higher risk,” Oetzel said.
While some studies don’t show long-term affects of subclinical hypocalcemia at calving, Oetzel said we’ve seen enough that we know for some cows there are negative impacts including an elevated risk for retained placentas, metritis, displaced abomasums, ketosis, and culling in early lactation.
“Subclinical hypocalcemia is detrimental to the average cow,” the veterinarian said.
To hear more of Oetzel’s recommendations about hypocalcemia, watch the webinar, “Calcium and the transition cow,” at www.hoards.com/WB_091420.